What is Pediatric Acute
Lymphoblastic Leukemia (pALL)?
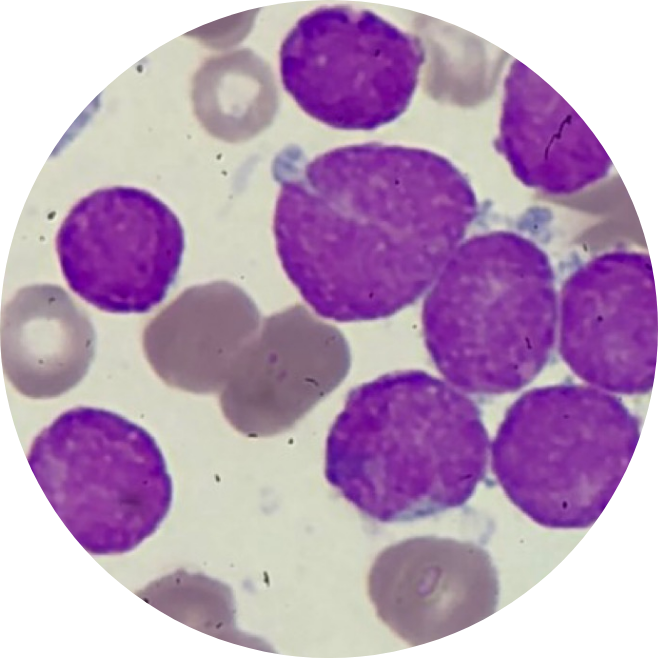
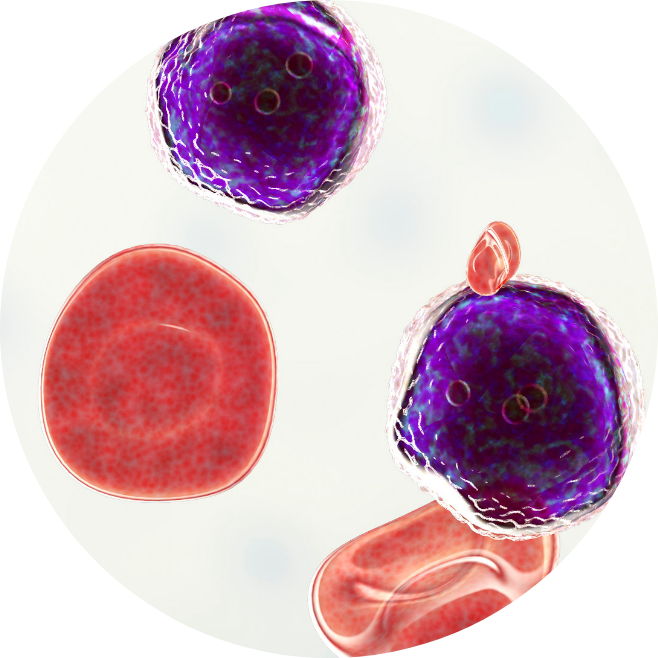
Pediatric Acute Lymphoblastic Leukemia (pALL) is the most common type of blood cancer diagnosed among children.1 In a child with pALL, the bone marrow makes too many lymphocytes, a type of white blood cell. When this happens, these cells fill up the bone marrow and stop it from making the usual amount of healthy blood cells. Thus, affecting the body’s ability to defend itself and putting the child at increased risk of infection.
“Acute” means that this type of cancer is aggressive in nature and usually gets worse rapidly if it is not treated immediately.
What is B-Cell Pediatric Acute
Lymphoblastic Leukemia (pALL)?
As part of the body’s immune system, B cells are natural defenders of the body. When B cells become cancerous, they can grow out of control and cause a type of blood cancer called B-cell pediatric Acute Lymphoblastic Leukemia (pALL).2
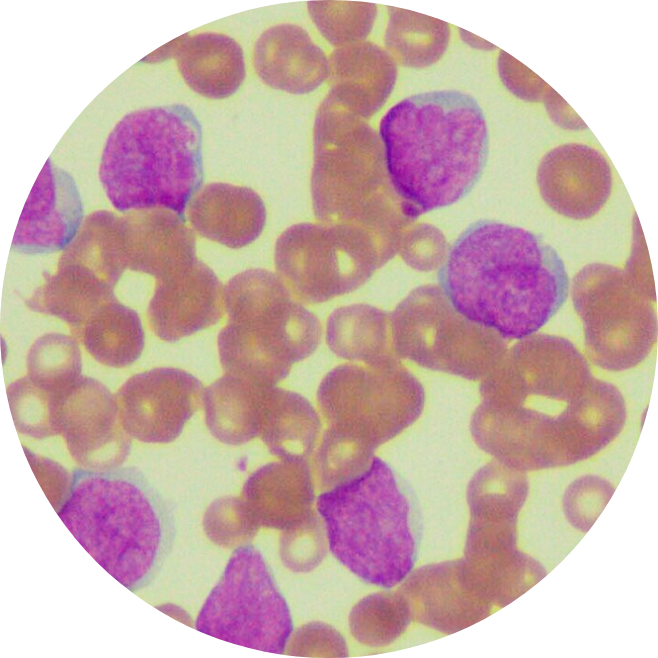
In pediatric Acute Lymphoblastic Leukemia (pALL) patients, abnormal cells in the bone marrow limit the production of red blood cells which carry oxygen, other types of white blood cells, and platelets. As a result, pALL patients may be anemic, more likely to get infections and bruise or bleed easily.3 While many children with pALL recover after their first treatment, some don’t.4
Did you know? According to World Health Organization (WHO), 55,767 cancer cases5 were diagnosed in Southeast Asian children aged 0-14 years old in 2020.
How is Pediatric Acute Lymphoblastic Leukemia (pALL) diagnosed?
To determine if a person has pediatric Acute Lymphoblastic Leukemia (pALL)6, the doctor will ask about the person’s medical history, the family’s medical history, followed by a physical exam to look for possible signs of the disease, such as swollen lymph nodes.
First, a blood test is drawn to check the blood cell counts, liver and kidney function. If the results show a high number of abnormal white blood cells, it could be a sign of pALL. Your care team may then refer you to a hematologist to help guide the next steps of treatment.
To confirm a diagnosis of pALL, a sample from the bone marrow is taken for further testing. Imaging studies, such as X-ray scans, CT scans, MRI, or ultrasound, may also be done for a better understanding of where the leukemia cells have spread.
What are the symptoms of Pediatric Acute Lymphoblastic Leukemia (pALL)?
The lack of healthy blood cells causes most symptoms of pediatric Acute Lymphoblastic Leukemia (pALL). Common Acute Lymphoblastic Leukemia symptoms to look out for include7:
- Pale skin
- Feeling tired and breathless
- Repeated infections over a short time
- Unusual and frequent bleeding (such as bleeding gums or nosebleeds)
- High temperature
- Night sweats
- Bone and joint pains
- Swollen lymph nodes
- Abdominal pain (caused by a swollen liven or spleen)
- Weight loss
- Bruises (or small red or purple spots) on the skin
In some cases, the affected cells can spread from the bloodstream into the central nervous system. Thus, causing neurological symptoms (related to the brain and nervous system), including headaches, seizures or fits, blurred vision, and dizziness.
What are the risk factors of Pediatric Acute Lymphoblastic Leukemia (pALL)?
Risk factors refer to anything that increases one’s risk of getting cancer, but they do not determine the diagnosis as Pediatric Acute Lymphoblastic Leukemia (pALL) patients may have few or no known risk factors. According to statistics, the risk for developing pALL is highest in children below 5 years old.19
Factors within your control
- Exposure to radiation, certain chemotherapy drugs and chemicals (such as benzene)
- Smoking
- Certain viral infections
- Genetic conditions (such as Down syndrome, Klinefelter syndrome, Fanconi Anemia, Bloom syndrome, Ataxia-telangiectasia, Neurofibromatosis, and Li-Fraumeni syndrome)
Factors outside of your control
- Age
- Gender
- Family history